Pericardiocentesis: What Does It Consist Of?
Pericardiocentesis is a procedure that involves the extraction of fluid from the pericardial sac using a fine needle. It owes its name to the pericardium, a kind of sac that surrounds the heart and is made up of two sheaths or layers. That is, it is a double membrane that surrounds the heart.
The tissue or membrane that makes up the fibrous pericardium (its outer part) is resistant and has a conical shape.
In addition, this layer is firmly attached to the diaphragm, through the pericardiophrenic ligament. In this way, the heart maintains its position despite changing body posture. In addition, it is also responsible for limiting the expansion or distention of the heart.
The serous pericardium (its internal zone) consists of two sheaths: the parietal pericardium and the visceral pericardium. In this case, the visceral layer is located directly above the myocardium (the heart muscle). However, the parietal layer is located on the inner aspect of the fibrous pericardium.
On the other hand, between these two envelopes there is a space called the pericardial cavity. In it there is a fluid that facilitates the displacement of the cardiac layers. Thanks to this lubricating fluid, the heart can carry out its movements normally.
How is pericardiocentesis performed?
- First, the medical team will select the place where the surgical procedure will be performed. As a general rule, it is carried out in the Intensive Care Unit or ICU. However, there are times when it is applied even in the patient’s room.
- Next, specialists will place an IV in the patient’s arm. In this way, they can give the patient fluids or medications if needed. They are usually recommended if an arrhythmia (sinus heart rhythm disturbance) develops. They can also be used in case of low blood pressure during the procedure.
- Later, the region below the breastbone will be cleaned and a local anesthetic will be applied. Therefore, the patient will not be bothered by the needle entry.
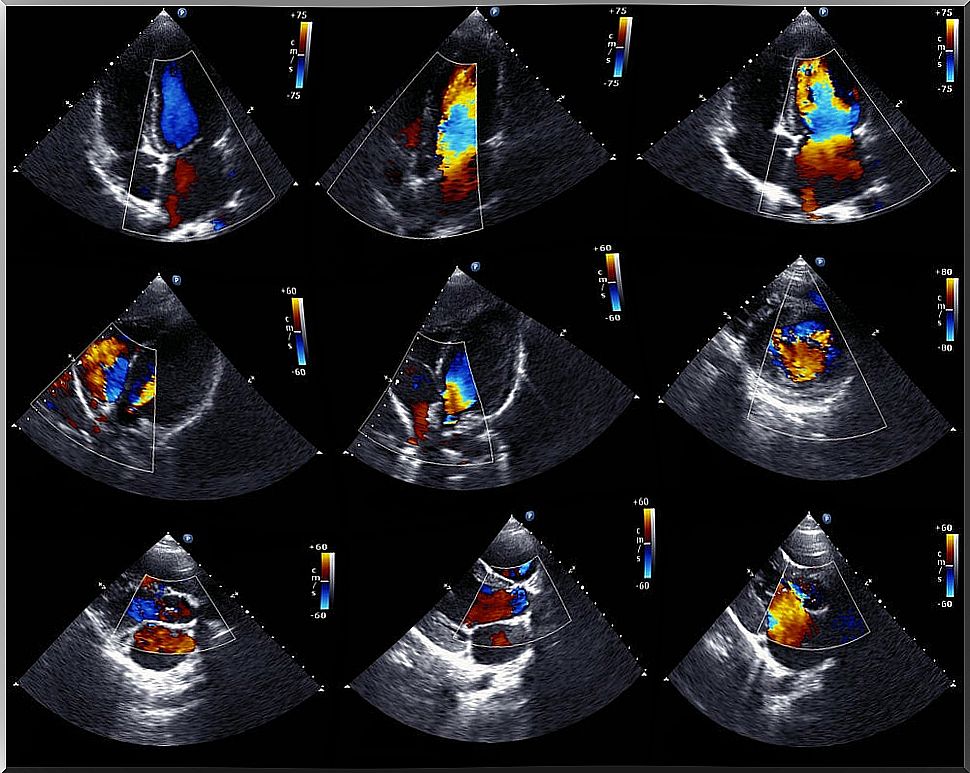
- Thus, with the help of an echocardiogram, doctors will guide the needle to the proper position thanks to ultrasound. Once correctly positioned, the needle is replaced by a tube or catheter. This is a small tube through which the fluid will drain into a small container.
- Often times, the catheter is left in this position to continue to draw fluid for several hours. During this medical method, the patient’s vital signs and how he responds to the operation will be monitored at all times.
- However, in case of complications, the medical team may decide to perform a surgical pericardiocentesis. In this case, the technique is more invasive and the patient must undergo general anesthesia to perform it. In it, you choose to drain the fluid into the abdominal or pleural cavity to remove it more easily.
Is preparation needed before performing pericardiocentesis?

Before the intervention, the doctor will tell the patient what measures to comply with, which are:
- Avoid drinking fluids during the hours before surgery.
- Avoid eating during the hours before surgery.
Additionally, the patient must sign a document indicating their consent to perform the operation and understanding of the risks involved. This is a normal legal procedure.
What can the patient feel?
Generally, the patient will feel pressure as the needle is moved through the chest. Likewise, there are patients who feel chest pain that can be counteracted with the use of painkillers.
In which cases is it recommended?
This medical examination of the pericardial fluid can be done for a number of reasons. For example, we can highlight the following clinical cases:
- Pericardial effusion. It is used to identify the cause of this disorder whether it is recurrent or acute. It consists of the accumulation of fluid in the pericardial cavity. This situation puts pressure on the heart and alters its functioning.
- Cardiac tamponade. Doctors choose this method also as a treatment for this problem which can be life threatening for the patient.